|
|
IN THE CORNER of Al Chin’s fourth-floor Silicon Valley executive office, one can barely see the surface of a large, round table beneath heaps of clutter: small bottles of crazy glue, plastic syringes, spools of yellow and blue tubing, needles, surgical pliers, glass test tubes. Chin, however, views this chaos differently. He sees the makings of life-saving medical devices. Nearly a decade ago, tinkering at his work table with a few of those odd items, the biomechanical engineer banged out the first prototype of an instrument now used in nearly 45 percent of coronary artery bypass operations nationwide. These surgeries reroute blood around blocked vessels in the heart by grafting pieces from long arteries or veins elsewhere in the patient’s body. Using Chin’s device — a foot-long, 0.4-inch-diameter tool called VasoView — surgeons can pluck out an entire leg vein, from the groin to the ankle, through several one-inch incisions. Today Chin — a slightly paunchy 51-year-old with deft hands — is looking toward a new frontier. Applying the same thinking that led to his VasoView invention, he is developing a tool that would give surgeons direct access to the heart through a single, similarly small incision. Chin envisions doctors using his device to implant pacemakers, treat atrial fibrillation — a dangerously irregular heartbeat — and perhaps one day inject stem cells to regenerate heart muscle. His mission might seem farfetched because in most heart operations, cardiac surgeons reach the fist-sized engine of life only after making a foot-long incision and cracking the patient’s breastbone. Chin’s experimental instrument, however, requires just one narrow cut below the sternum to begin its path to the heart. In test operations on 200-pound pigs, Chin has used the blunt-tipped, rod-like instrument to burrow through fat and track along blood vessels. Yet the tool is gentle enough to nudge, but not puncture, the exquisitely thin sac, or pericardium, that surrounds the heart. The instrument’s smooth, stainless steel exterior hides its most critical feature: a tiny, 0.2-inch-diameter telescope, or endoscope, that connects to a digital camera. The camera projects high-resolution images — what the scope “sees” inside the body — onto a TV monitor near the operating table. This arrangement allows surgeons to clearly view where the instrument is going without laying the chest open. Since the 1970s, doctors have used endoscopic devices, also known as “keyhole” surgery tools, elsewhere in the body — to help remove the gallbladder from the abdomen, for instance. Tampering with vital organs, however, carries a much greater risk. A single wayward prod of the heart can cause life-threatening disruptions in the force or rhythm of its beating. A patient can die in minutes. Nevertheless, keyhole heart surgery procedures started gaining popularity in the mid-1990s. The new technology promised to ease patient pain, reduce the risk of infection, and shorten postoperative recovery time. Patients could get back on their feet within weeks instead of months. However, among cardiac surgeons, keyhole techniques remain far from mainstream. In 2002, only about one in four heart operations in the United States used minimally invasive tools. Although far less painful than standard operations, keyhole procedures pose a formidable challenge for heart surgeons, who must sew grafted vessels into place and perform other precise manipulations on a critical organ through just several tiny holes. But Chin is accustomed to penetrating difficult and uncharted territory. Holding 141 U.S. patents, he is the “designated inventor” and vice president of research at the Santa Clara, Calif., branch of Guidant Corporation, which develops vascular and cardiac surgery tools. His knack for inventing emerged over 40 years ago. As a fifth grader, Chin took apart ballpoint pens and fitted them with contraptions for shooting paper wads across the room, or with tiny plungers so they could blast out water like a squirt gun. As a junior at the Massachusetts Institute of Technology in the early 1970s, he took third place in a student innovation contest by designing a pedal-powered snowmobile. “I’d always made things with my hands,” Chin says. “But I didn’t realize until college that this ability was actually design.” He went to Stanford University, near Palo Alto, Calif., to earn a mechanical engineering master’s degree. Even when he ended up on “the project nobody wanted” — building a device to carry a 500-pound piano up stairs — Chin crafted the winning blueprint. The best designs, he says, are simple and practical. “If you have 500 pounds and you want to walk it upstairs, the last thing you want to have happen is dropping it,” Chin says. “You don’t want to lose your balance going up the stairs.” His piano mover consisted of two connected tables that could slide and rotate with respect to each other, with one remaining planted as the other maneuvers up the next few stairs. After completing his engineering degree in 1976, Chin decided he was sick of school and started working at Hughes Aircraft Company in Fullerton, Calif. He spent a year there, making laser weapons to shoot down planes, but “it only took me a week or two of going into work to see that this was really boring,” Chin recalls. “You’d have these rows of 50 to 80 engineers in a big room. All I remember was, they were looking forward to coffee breaks and weekends. In 20 years, I didn’t want to be one of those guys.” Instead, Chin spent a good chunk of the next 20 years catapulting himself into a new field: medicine. His interest was piqued by conversations with his brother-in-law, who was doing an internship in internal medicine at the University of Southern California in Los Angeles. “The ability to work with patients was something that really seemed worthwhile,” Chin says, “much more so than completing a doctorate in mechanical engineering.” He decided to go back to Stanford for premedical coursework and then apply to medical school. But Chin had no intention of abandoning his love for inventing. “I knew that if I wanted to get into medical school, I should do something extraordinary,” says Chin. His undergraduate grades, he says, were “iffy” at best, but he was good at design, so he started calling surgeons to ask if he could build medical devices for them. By the time he submitted his application for medical school at the University of California, San Francisco, in 1978, he had already filed five or six U.S. patents for components of a device that can help surgeons remove fatty or calcium deposits from partially blocked arteries. Chin got into UCSF. After completing his M.D. in 1983, followed by two years of a general surgery residency, he had amassed enough academic knowledge and practical experience to fuel a slew of clinical innovations. He spent the next three years working with Stanford surgeon and medical device designer Thomas Fogarty, before founding his own startup, called Origin Medsystems, in 1988. Origin was later acquired by pharmaceutical giant Eli Lilly and spun off into Guidant in 1994. 
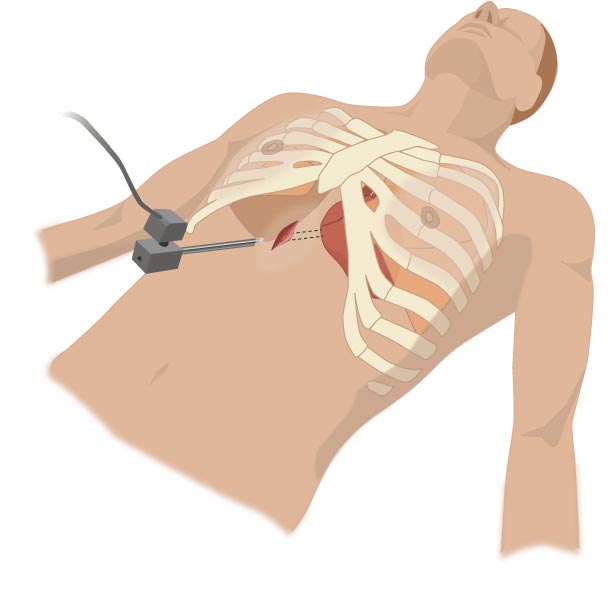
MOST MEDICAL DEVICE INVENTORS typically think of an idea, sketch it out, and go through a lengthy series of consultations with machinists, technicians and physicians before eventually building a prototype. But because of his cross-disciplinary training, Chin can bypass many of the intermediate steps in that process. “If I get a concept,” he says, “I’ll go and make it myself.” Chin doesn’t bother with sketches. Usually a picture of a new device just pops into his head, he says. He’ll go straight to the machine shop, three stories below his office, and make the gadget. “Then I’ll test it,” he says. “If it works, I’ll go back and draw it up and submit a patent application.” Often it’s these kinds of quick, bang-up prototypes that get the nod. Though usually quite different from the final product, these models provide the foundation for developing new devices. John Lunsford, an engineering manager at Guidant, says he always encourages his team members to make “Al Chin” prototypes. “They’re not the prettiest, not the most marketable or well-rounded, but they work and they prove the concept.” Simplicity remains a cornerstone of Chin’s inventing. Although designs appear in his mind almost ceaselessly, few make it to the machine shop. He often starts with four or five different approaches when he conceives a new tool, but in order to beat his competitors to the market, Chin says he’d “better come up with a device that’s simple enough to be adopted by the practicing clinician with minimal teaching.” Devising user-friendly prototypes isn’t usually easy, as Chin’s experience with VasoView shows. Back in 1995, he pioneered that device — which would pave the way to quicker, less painful coronary bypass operations — by taking a foot-long, glass tube from his office work table, attaching a tiny endoscope inside one end, and hooking it up to a digital camera. Operating on pigs, Chin could stick this tube through a one-inch incision in one leg and carefully thread the gadget up along the outside of the vein. The endoscope worked beautifully: Chin could see exactly where the probe was going. However, when he put it to its next test — surgery on human cadavers — he realized a critical flaw. “When I got into the cadaver, there was so much fat that I couldn’t see a thing,” Chin recalls. His strategy for solving this visualization problem came from a textbook that described early attempts at using an endoscope to see the heart during keyhole surgery. In particular, Chin recalls reading about English and Japanese surgeons who in 1943 had placed a scope inside of a condom-sized, transparent balloon to look inside the heart. Once the doctors inflated the plastic balloon, they could use the endoscope to “watch” through its stretched membrane. The balloon kept the scope lens from rubbing up against fat and bloody tissue that would obscure its view. Adapting the same idea to his own device, Chin reasoned that as long as nothing obstructed the lens of the endoscope, the device should work, because it would allow the surgeon non-stop visualization. Bingo. “All of a sudden it came to me,” Chin says. “What if I made something that had a conical tip that was transparent? I wondered if the tip could not only dissect but also visualize continuously. Those two principles I knew were important.” Chin tinkered more with his initial glass tube prototype, this time covering the end that pokes into the body with a protective nose cone. He made the conical tip out of polycarbonate plastic so it would be transparent and rigid, like swimming goggles. With the endoscope tucked about a centimeter behind it, the cone’s blunt outer tip allows it to dig through fatty connective tissue without spearing the vein. “When you push it along the vein, it separates the vein from the surrounding soft tissue automatically,” Chin says. “You watch and dissect at the same time.” CHIN HAS BEEN APPLYING this same strategy to his new heart tool. It resembles VasoView, but its main probe abuts a second, shorter tube — like disposable chopsticks before they’ve been separated. The instrument’s primary rod houses the endoscope, enclosed by the VasoView conical tip, and performs the “watch and dissect” function. The adjoining second tube provides an 0.4-inch-diameter “working port” through which the surgeon can insert accessory instruments — such as small tools for cutting and grasping — to perform finer manipulations once the device has reached the heart. To demonstrate, Chin opens a PowerPoint presentation on his desktop computer and clicks on a video that shows him using the device to operate on an adult pig. In the film, after inserting the blunt-tipped device through a one-inch incision below the animal’s ribcage, he plunges it through the diaphragm and pokes through fatty tissue that surrounds the heart. “It only took me a couple of minutes to get in,” Chin recalls. After gently bumping the heart with the instrument, he threads his accessory tools through the device’s working port to grab the edge of the pericardium and snip a little hole. In the video’s final moments, Chin carefully directs the tool through the hole and uses the instrument to sweep underneath the heart, then to each side, then all the way around it — showing he can access all parts of the organ through a single small incision. Chin’s hope is that his heart tool will eventually be used to perform certain procedures on an outpatient basis. “Patient comes in, we do a procedure, fix the heart, patient gets out,” he says. “They won’t have to stay overnight in the hospital.” For the most common cardiac operation, coronary artery bypass, Chin predicts his access device will trim three to five days from the typical five- to 10-day hospital stay. The new instrument would also reduce the risk of stroke and other complications associated with the standard procedure of using a heart-lung machine, he says. Alternative methods of keyhole heart surgery offer similar benefits, but even the most state-of-the-art techniques seem ruthless compared with Chin’s. One current strategy uses several small incisions: Surgeons reach the heart by inserting multiple catheters through the ribcage. This mode of entry requires the doctor to collapse the patient’s lungs — a predicament avoided by Chin’s tool, which gains access to the heart from below the ribcage. Cardiac surgeons who have tried a variety of minimally-invasive devices praise Chin’s invention for its simplicity and versatility, saying it is the only one that allows access to the heart through a single port, does not require a lung collapse, and could be used under local anesthesia. “It has the potential to be the hands-down winner,” says Dan Beckman, a cardiac surgeon at Methodist Hospital in Indianapolis who consults for Guidant. So far Chin and others have used the device in over 125 pig surgeries and about a dozen cadaver procedures. The instrument earned FDA clearance over a year ago. But before it hits the market — next year, Chin hopes — the tool must undergo extensive in-house development at Guidant. After a device leaves Chin’s realm, other engineers fine-tune its design to expedite manufacturing. They also test the tool for durability and compatibility with human tissues. And the marketing department must fully document the results of all lab and animal testing of the new tool. In the meantime, Chin spends his Fridays hunched over anesthetized pigs atop operating tables at a privately owned Berkeley animal facility, eager to demonstrate his cutting-edge tool. He shows his tools to visiting surgeons. He teaches R&D engineers how to use the technology they’re developing to operate on pigs. He trains the Guidant sales force. Occasionally he brings in local bioengineering students from Stanford University. “One of the things we love about Al is he’s so approachable,” says Liming Lau, a project group leader in cardiac surgery at Guidant. A few years ago, Chin even invited his YMCA trainer, Ondria Follett, to observe a pig surgery. “I was really intrigued by the procedures Al had developed,” says Follett, who once worked as an assistant in a gynecology office. “He’s a genius, and he’s so humble.” Explains Chin, “You can’t get an understanding through a description. You have to see it.”
Indeed, seeing is everything in his line of work. A decade ago,
Chin recognized continuous visualization as the critical feature
that would propel VasoView into surgical stardom. Today some
colleagues say he’s a visionary for imagining that similar
technology could be applied to reaching the heart. “He
sometimes thinks way ahead of the game,” says Marco Zenati, a
cardiac surgeon at the University of Pittsburgh Medical Center.
“In five years, he will be a hero for this.” |