|
| Illustration: Kirsten Huntley |
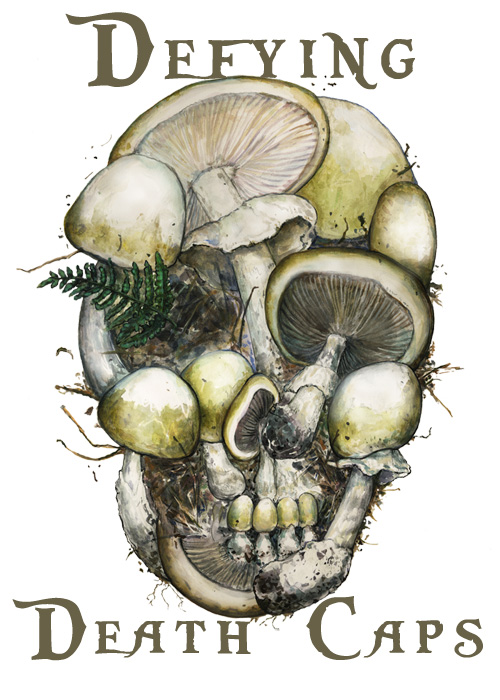
A doctor fights to gain approval for an antidote to a deadly poison. Elizabeth Devitt tracks the battle. Illustrated by Kirsten Huntley and Tanya Young.
Appearances can be deceiving. For mushroom foragers, they can also be deadly.
One of the world’s worst poisons comes in a small, delicious package: the white-capped Amanita phalloides. This modest-looking mushroom often grows alongside chanterelles and porcinis, the favorites of many a chef. The “death cap” also looks similar to tasty mushrooms common in other countries. But if foragers mix up this mushroom with other fungi, eating just one might be the last mistake of their lives.
Six years ago, a family of six in Watsonville, California, learned about Amanita toxicity the hard way. Hours after enjoying a meal with mushrooms picked at a local park, they suffered vomiting and severe diarrhea. By the time they arrived at Dominican Hospital in Santa Cruz and described their dinner to Dr. Todd Mitchell, they were in deep trouble. Although Mitchell had never treated mushroom-poisoned patients, he knew their livers were under attack. He didn’t yet know there was no antidote to save them — at least, not anywhere in the United States.
“Well, they weren’t going to die on my watch,” says Mitchell.
After a quick Google search, he discovered European physicians had been treating poisoned patients with an intravenous extract of milk thistle seeds made by a German company. He also learned the U.S. Food and Drug Administration (FDA) had never licensed the medication, called Legalon SIL, for use in this country. No U.S. doctor had permission to import the world’s only antidote to the death cap poison. But that didn’t deter Mitchell, who hunted down every key company and official necessary to get the drug couriered to California on a last-minute plane flight.
Eleven days later, all but the eldest family member were recovering at home. Although Legalon SIL revived the grandmother’s failing liver, the toxic episode overwhelmed the rest of her body. She died, one of the mushroom’s 12 victims in the state since 2006.
Now, Mitchell is wrapping up the only U.S. clinical trial for the antidote to the poison, known as amatoxin. His three-year study enrolled more than 60 patients. So far, nearly all of them have survived. His results might rewrite the tragic endings of mushroom toxicity stories.
Many patients survive without the antidote. They recover after large doses of intravenous fluids and treatment for vomiting and diarrhea. But some people spiral downward into liver failure. Mitchell has found the milk thistle extract can save those patients, as long as their kidneys haven’t yet shut down from severe dehydration. With early antidote treatment and intensive fluid therapy, the liver can overcome the mushroom toxin’s assault.
But Mitchell still must convince the FDA — and many of his colleagues — that milk thistle extract is key to surviving the death cap’s deadly ingredient.
Tempting toxin
The “death cap” is different from other members of its fungal family. Most mushrooms associate with specific tree roots; porcinis pop up near pine trees and chanterelles cozy closely with oaks. Amanitas aren’t nearly so choosy.
A native of Europe, researchers believe the Amanita phalloides disembarked in Monterey harbor with a shipment of oak trees in the 1900s and has progressively invaded other parts of the country. Now it flourishes under West Coast oaks, East Coast pines, and even redwoods. Foragers have found them in the Midwest and Texas, too.
 |
Illustration: Tanya Young |
|
|
The death cap has two sister species that also are lethal: Amanita ocreata, an American native, and the East coast Amanita bisporigera — nicknamed “avenging angel.” Other Amanitas are safe to eat. Only two other mushroom species, Lepiotas and Gallerina, make deadly amatoxins.
Unlike other poison pushers found in nature, none of these deadly fungi look dangerous or come with bitter-tasting warnings. “They’re extremely attractive
mushrooms — they just look like they’d taste good — so they can be a real threat,” says David Campbell, an expert who has identified mushrooms for the California Poison Control System for more than two decades.
That appetizing appearance got Frank Constantinopla in trouble. The Virginia resident couldn’t resist picking the bounty that burst all over his yard after heavy rains two Septembers ago. “I thought they were the same as I always picked at home,” says the Philippines native. The white-capped visitors looked like perfect ingredients for a stir-fry. “They tasted really good.”
Hours later, Constantinopla said he “felt his stomach acids running through his body.” Although he suspected the mushrooms were the cause, he expected his diarrhea symptoms to go away. Instead, he got sicker.
Toxic travels
The amatoxin had begun to work its wicked ways. It’s so hardy that digestive enzymes in the mouth and stomach don’t affect it. Then, it slips through the intestinal wall and gets absorbed into the bloodstream. Everything that enters our blood from our intestines first travels to the liver, the detox center of the body.
There, most of the amatoxin gets pushed out; two-thirds of the poison payload goes to the kidneys, which flushes it out of the body in urine. But even if the kidneys do their job, the problem is the one-third that stays behind. It sneaks into liver cells by binding to a transport protein that cells allow to pass through. Then the real trouble begins. Our livers survive most toxic assaults because they can regenerate by making new cells. When amatoxin arrives, it shuts down this system by binding to an enzyme that normally allows each liver cell to order DNA and rebuild.
|
|
Illustrator Kirsten Huntley animates the effects of Amanita mushroom poisoning inside our bodies. |
|
|
A cruel twist of biological engineering brings more poison back to the liver. Most metabolic pathways try to conserve and recycle. When the liver breaks down nutrients or toxins, it sends them back into the bloodstream. These byproducts are often packaged with bile, or other biological escorts, to help the body use or eliminate them. Then, some of those escorts circulate back to the liver. Amatoxin binds to bile, returning to launch another attack on liver cells. If nothing interrupts this cycle, every cell in the liver gets destroyed.
Without an antidote, says Mitchell, the best possible outcome is sobering: a liver transplant, a lifetime of medication to preserve the new liver, and a seven-figure hospital bill.
Constantinopla was lucky. After three days of relentless retching and diarrhea, he went to an emergency room. When blood tests showed his liver wasn’t working well, the doctor told him “we’re crossing our fingers for you to recover.” His relatives already had visited. At the time, he didn’t fully understand why they were all crying or why they called his mother, still living in the Philippines.
An ambulance rushed Constantinopla to the MedStar Georgetown University Hospital, a facility renowned for its expertise in transplant medicine. His doctor promptly put his name on the list for a new liver. She had never treated a mushroom-poisoned patient, but a colleague gave her Mitchell’s contact information.
“She told me there was a drug, but it was not yet approved,” says Constantinopla. “I knew it was a gamble, but I signed the papers right away.” The hospital soon received Legalon SIL from an East Coast repository in Pittsburgh.
By the following weekend, Constantinopla was cooking at home again, although he swore off mushrooms forever. “I know they’re not all bad,” he says, “but I want everyone to know not to eat mushrooms if they don’t know what they are.” The sound of ambulance sirens still reminds him of the hymn Amazing Grace.
Super seeds
The milk thistle, a tall weed with spiky leaves and a lavender flower, doesn’t look like a death-defying hero. But it’s been touted as a liver health remedy since ancient Roman times.
 |
Illustration: Tanya Young |
|
|
The active ingredient, silibinin, takes the same “taxi” into liver cells that amatoxin needs. By commandeering all the cabs, silibinin stops the toxin from getting into liver cells. The extract can also prevent poisonous effects inside cells. It blocks amatoxin from triggering cell-killing signals, and it kick-starts the liver’s cell machinery to make proteins for repairs.
In Europe, where mushroom foraging is a cultural tradition, Legalon SIL has been available for decades. The intravenous medicine is licensed for use in more than 20 European countries, says Joe Veilleux, president of the American office of Madaus USA, the manufacturing company. “In the past, when other people called for the drug, they hung up when they found out we didn’t have it in the country,” he says. “Mitchell didn’t let it end there.”
After Mitchell saved the Watsonville family in 2006, it took yet another emergency to gain attention from the FDA. This time, a woman and her twin grandsons ended their mushrooming foray in a San Francisco hospital. “It was like lightning in a bottle, again,” says Mitchell, of his second last-minute scramble to get Legalon SIL into the country. Everyone survived, and Mitchell earned FDA approval for a clinical trial with the antidote.
Previous studies in people were based on after-the-fact reviews of medical reports from poisoned patients. The challenge with running a bona fide clinical trial for amatoxin was following the standard protocol: a double-blind study in which one group gets treated with the drug under investigation, and the other group either gets a placebo or the current “standard of care.” No one is supposed to know who gets which treatment.
“But this is a life-threatening situation,” says Veilleux. “You can’t give someone who’s dying a sugar pill.” The situation for silibinin, argued Mitchell, was similar to a previous hospital trial for an antidote to cyanide poisoning. In that trial, only people who ingested cyanide got the experimental treatment. That paved the way for Mitchell’s trial to begin. In 2009, Dominican Hospital in Santa Cruz began enrolling patients.
The other difficulty was the rarity of poisonings, says toxicologist Alan Buchwald of Dominican, sub-investigator for the clinical trial. Only 59 Amanita cases were logged in the state between 1997 and 2009, according to records from the California Poison Control Service.
“The real problem is that most primary physicians have no experience with it,” says Buchwald. Only 10 percent of all reported mushroom cases are fatal. However, 90 percent of those fatalities are caused by amatoxin. If patients don’t get treated within four days, their odds of survival plummet.
Antidote antipathy
Mitchell is now preparing a journal article describing his trial results from treating 61 patients with silibinin. So far, his data show that every patient getting Legalon SIL recovered from Amanita poisoning — provided that they did not go into kidney failure before getting the drug. When asked to comment, FDA officials refused, as they still consider the clinical trial active.
But even before Mitchell's paper comes out, not everyone is convinced the antidote makes much difference.
“I have a list as long as my arm about antidotes and treatments proposed over the years,” says Kent Olson, medical director of the San Francisco division of the California Poison Control Service. “Milk thistle seems promising, but like other treatments we’ve used, some people who were really sick got better on their own. I have a natural skepticism about an antidote that hasn’t undergone controlled studies.”
Although Mitchell’s trial is the first one for people, several double-blind studies on dogs more than two decades ago showed silibinin was effective in saving their livers from amatoxin. But Olson, who wrote a textbook on toxicology and poison, notes the experimental dogs were treated with antidote within six hours of poisoning. In real life, the toxin takes at least that long to make someone sick. Most victims don’t show up at hospitals until many more hours — or even days — have passed.
 If someone calls the poison control center with symptoms suggesting they ate death caps, Olson says physicians rely on clinical experience and test results to decide how best to treat patients. Although there’s a urine test for dogs, there’s no reliable test to prove a human patient suffers from amatoxin. If doctors want to try the experimental antidote, Olson said the poison control center can provide a referral to Mitchell for the drug. If someone calls the poison control center with symptoms suggesting they ate death caps, Olson says physicians rely on clinical experience and test results to decide how best to treat patients. Although there’s a urine test for dogs, there’s no reliable test to prove a human patient suffers from amatoxin. If doctors want to try the experimental antidote, Olson said the poison control center can provide a referral to Mitchell for the drug.
Statistics from Europe don’t support Mitchell’s cause, says Michael Beug, toxicologist for the North American Mycological Association (NAMA). There, milk thistle is considered the standard of patient care. However, death rates from amatoxin still hover at 20 percent. Without the drug, only 10 percent of patients in the U.S. die from death caps, according to a three-decade review of NAMA reports Moreover, the Medical Journal of Australia recently reported four deaths in a review of ten Amanita patients treated with Legalon SIL from 1999 to 2012.
Mitchell contends that such mortality rates don’t reflect the effectiveness of milk thistle. He attributes most patient deaths to lack of aggressive supportive care. Moreover, he says, the treatment doesn’t endanger patients in any other way. He’s optimistic the FDA will approve its use in the U.S.
Once Mitchell submits his results, approval should take less than ten months under current FDA guidelines for an "orphan drug" — meaning it is not intended to treat more than 200,000 people. Even if the milk thistle extract doesn’t win approval, Legalon SIL won’t be banned from hospital use. The drug can still be used as an investigational drug as long as no safety issues arise and the German manufacturer wants to continue making it available, says Sally Loewke, an FDA representative from the Office of New Drugs.
Treatment protocols may differ, but no one has argued to ban the thistle extract. As Beug says, “I don’t know what I think about the [research] statistics, but I’d certainly want to have them use the stuff on me.”
Sidebar: Transgenically Modified Poisonous Mushrooms
Most foragers avoid Amanita phalloides, but one man makes special trips to northern California to collect them. He has to. They won’t grow inside his lab — or anyone else’s.
 |
Author Liz Devitt explains how to identify deadly Amanita mushrooms in this narrated slideshow. (Click image to launch YouTube video.)
|
|
|
“That’s just one of the problems with Amanita. It’s extremely finicky about when it decides to fruit,” says plant biologist Jonathan Walton of Michigan State University. He earned his undergraduate degree at UC Santa Cruz, a campus well-populated by Amanita. Today, Walton devotes much of his time to tinkering with the mushroom’s toxins. He’s trying to turn their poisons into potential medical treatments.
The main toxin of poisonous Amanita mushrooms, called amanitin, has a peculiar chemical structure: a protein made of two rings of carbon-based octagons. This puts it in the company of other exceptionally potent biological compounds, says Walton. Some of them are good, such as penicillins; others are wicked.
Six years ago, Walton’s lab figured out that Amanita phalloides uses a one-step process to make its toxin. The poison needs a sequence of eight amino acids transcribed by ribosomes, the cell’s protein factories, directly from DNA. While this is standard operating procedure for most genetic material, it’s not the usual path to poisons in fungi. Other mushrooms use special enzymes, called nonribosomal peptide synthetases, to make the building blocks of their toxins. Then, they use additional enzymes to assemble those ingredients into an active poison.
The way Amanitas make their poison is incredibly efficient, says Walton. He's fascinated by the simple production system, which makes the toxin vulnerable to manipulation. Changing one tiny section of the gene could create a new toxin. That modified compound might kill rapidly dividing cells — like cancer cells — yet leave a person unharmed.
There are millions of permutations of the eight amino acids that make amanitin, so there could be hundreds of novel compounds, Walton says. Some could have beneficial effects. He’s collaborating with a cancer biologist, a tuberculosis specialist, and an expert in antibacterial resistance to test his new compounds.
“Transgenically modified poisonous mushrooms,” says Walton. “It could sound pretty creepy.” But the danger is minimal: The mushrooms refuse to grow in the lab, and the minuscule amounts of toxin get tested only on cell cultures. Although the work is arduous, the payoff could be big. The National Institutes of Health has funded Walton’s lab with more than $1 million to explore the possibilities.
So far, Walton has prodded novel genes to make different molecules. Next, he’ll try to make a modified toxin. He already knows which amino acids he wants to swap out first. “Then we’ll try stranger and stranger things,” he muses.
Story ©2013 by Elizabeth Devitt. For reproduction requests, contact the Science Communication Program office.
Top
Biographies
 Elizabeth Devitt Elizabeth Devitt
B.A. (zoology) University of Vermont
D.V.M. Tufts University School of Veterinary Medicine
Internship: Nature Medicine (New York)
I was the quintessential little girl who loved horses. I didn’t want Barbie dolls; I wanted Breyer horse models, riding boots, and every equine book ever written.
When I grew up, I broadened my horsey horizons to become a veterinarian. I was sworn to protect public health and licensed to heal every species—except our own. That vast territory of veterinary medicine once felt boundless to me. Now, growing conflicts among animals, man, and the environment threaten the well-being of us all, and I feel limited by my profession. I want to have more global impact.
Journalism, my other lifelong love, was the perfect solution. As a writer, I plan to hoof it around the world and use my medical history to find the science stories that might create our healthier future.
Elizabeth Devitt web site
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
 Kirsten Huntley Kirsten Huntley
B.A. (art and archaeology) Princeton University
Certificate (visual arts) Princeton University
Internship: Amadeo Bachar
Kirsten Huntley grew up in Los Angeles. She won the Francis LeMoyne Page Award for her fine-art thesis in painting and printmaking at Princeton. Her professional experience includes working for Christie’s Auction House, Young & Rubicam, the Los Angeles County Museum of Art, the Getty Museum, the L.A. Natural History Museum, the La Brea Tar Pits and UCLA, with a focus on print design, web design and creating visual representations for complex information and systems. She is proficient in traditional and new media, including oil paint, pen and ink, gouache, watercolor, and Adobe Creative Suite.
Kirsten’s work has a fresh and graphic edge. As an observationalist, she combines a keen eye with her extensive background in design and technology to create innovative ideas to best convey information and satisfy her clients’ needs. Kirsten has exhibited in Los Angeles, Connecticut, Pont-Aven, France and New York, and she ran a pop-up gallery in Little Tokyo, Los Angeles. Currently, she is a freelance illustrator and designer.
Kirsten Huntley web site
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
 Tanya Young Tanya Young
B.F.A. (painting, photography) The School of the Art Institute of Chicago
M.F.A. (painting) University of Michigan, Ann Arbor
Internship: Scripps Institution of Oceanography (La Jolla)
After training and working as a painter, I decided to expand my career and enter the field of science illustration. After all, my inspiration has always come from the natural world and Earth’s phenomena. Art-making is one of most basic human impulses, like singing and dancing. In science illustration, art-making is also an important communication tool, which can convey the mystery and excitement of science, tell the story of discoveries, make comparisons, or explain a process in a way which will be useful to a scientist, student, or anyone who loves things beautiful and interesting!
Tanya Young web site
Top |