
|
| Illustration: Justine Shih |
Traces of the toxic metal loiter in our homes and our bodies, and we don't fully understand its risks. Meghan D. Rosen mines for details. Illustrated by Justine Shih. |
 |
Dark drops of blood seep from the tip of my baby’s tiny outstretched finger. They well from the pinprick, cling to her skin, and wobble briefly before a nurse scrapes them into a clear plastic collection vial. The vial is small—about the size of a pen cap—and we need only a dozen drops of Briar’s blood to fill it.
We were lucky this time; we got a good stick. We’ll go through the whole procedure again next year, when Briar is two. She’s not sick, she’s not developing abnormally, and there’s nothing wrong with her physically. But we live in an apartment built before 1978, the year lead was banned from household paints. For kids who live in homes like mine, the blood test is a routine screen for lead poisoning.
Lead in the air and the soil can steal into our bodies through a breath, a touch, or a taste. In the past few decades, federal regulators have tried to scrub the metal from our blood and bones by cutting out common sources of contamination. They’ve mostly succeeded. The switch to lead-free paints and gasoline cut national blood lead levels to less than one-quarter of what they had been.
 But thousands of tons of lead spewed from tailpipes and industrial plants still pollute our landscape—and it could linger for centuries. Recent research also implicates lead for social disorders and drops in IQ. Even minuscule amounts can stunt a child’s development. But thousands of tons of lead spewed from tailpipes and industrial plants still pollute our landscape—and it could linger for centuries. Recent research also implicates lead for social disorders and drops in IQ. Even minuscule amounts can stunt a child’s development.
In January 2012, mounting scientific evidence against lead propelled a federal panel into action. It urged the U.S. Centers for Disease Control (CDC) to lower the threshold for lead poisoning. Four months later, the CDC adopted the stricter standard, reclassifying hundreds of thousands of U.S kids into a newly defined danger zone.
“People like to think all the lead in the environment has gone away,” says UC Santa Cruz environmental toxicologist Russ Flegal, who has studied trace metals since the 1970s. “Well, it hasn’t. It’s a chronic problem.”
Heavy metal
The world’s largest concentration of lead ore rests in the southeast corner of Missouri, where thick bands zigzag through the mining district. Metallic lead is rare—it’s usually mingled with copper, zinc, or silver—so smelters refine ore to free the metal from the rock. They crush it, roast it, and melt it in blistering blast furnaces that layer the molten metals by density. Lead sinks to the bottom, and everything else is skimmed off the top. All the while, metallic vapors escape from each smelter’s smokestacks.
The purified metal has a gleaming chrome luster that tarnishes to a muted grey. It’s heavy, soft, and easy to melt, a near-perfect combination for metal work and weaponry. Bullets, plumbing, batteries, and radiation shields all exploit lead’s heft and utility. Until the 1980s, it was regularly added to gasoline to boost octane ratings and lubricate engines. But centuries of use have exposed the costs of smelting and the dangers of lead exposure, especially to children.
Our understanding of lead’s effects on kids has shifted from outright denial in the early 1900s to wary acceptance in the 1970s. We’ve dialed back the amount of lead that’s considered safe from 60 micrograms per deciliter of blood (mcg/dl) in the 1960s to 10 in 2011. The new standard slices that number in half. Today, the national average in our blood is 1 to 2 mcg/dl. But there’s no amount of lead in the body—not even a speck—that scientists can agree is harmless. And there are no people who are completely free from its touch.
Lead, lead everywhere
Traces of lead appear throughout Flegal’s clean and orderly office. It rests on his bookshelf, settles on his desk, and covers his walls. Black letters emblazon the word ‘L-E-A-D’ on a coffee mug, and framed covers of scientific journals highlight a career spent tracking toxins in the environment. But a focal point is a black wooden frame on the wall across from his desk. It’s divided into a 3x3 grid, with nine slots for pictures. Each showcases a product once contaminated with heavy metals. In most, the culprit was lead.
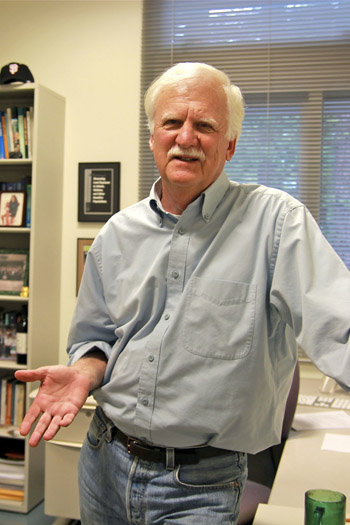 Photo: Meghan Rosen
Photo: Meghan Rosen |
UC Santa Cruz toxicologist Russ Flegal.
(Click on image to see larger version) |
|
|
Flegal, a tall, trim man with a neat white mustache, calls it his trophy case. He’s been an expert witness for the state of California in dozens of cases. “I’m always doing it,” he blurts out. “It’s horrible!” Environmental lawyers come to him with suspicious products, his lab workers test how much lead they contain, and then he testifies. Some sources of lead in the photos are obvious; one of them is the Shell oil sign. Others are surprising. His lab has found lead in calcium pills, chocolate, and balsamic vinegar. “It’s actually easy to measure lead in consumer products,” Flegal says, “because the amount is so high.” But lead can taint non-food items, too. Key makers once used lead as a lubricant while punching out pieces of brass, and lead from crystal goblets can leach into wine in minutes.
Courtroom battles between manufacturers and public health advocates trimmed lead from these products. And in 1986, Proposition 65 passed in California, requiring businesses to tell customers before exposing them to chemicals that might cause cancer or birth defects. So you can still buy lead crystal wine glasses—and even decorative pacifiers and baby bottles—but not without a warning sticker.
“I’m leery of products that aren’t regulated,” Flegal says, “especially herbal products.” Many are imported from countries that use leaded gasoline, a major global source of contamination. Though the U.S. Environmental Protection Agency (EPA) outlawed leaded gas for highway driving in 1996, it’s still legal for boats, airplanes, race cars, and off-road vehicles. But 16 years of cleaner fuel hasn’t been enough to purge the metal from our environment.
City of lead
Some of that lead lingers in unexpected places. Because air pollution drifts back down to earth, forests harbor traces of industrial metals in their soil and trees. The toxins stay put until fires or floods sweep them away.
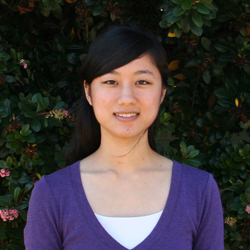
Graduate student Kingsley Odigie in Flegal’s lab recently measured the lead in ash from a 2009 wildfire in Santa Barbara County. “We wanted to see how much lead could be removed from the forest after a fire,” Odigie says. All but two of his samples were contaminated with lead. Santa Barbara isn’t a mining town, and compared to other Southern California cities, it’s practically pollution-free. Where did the lead come from?
 Photo: Meghan Rosen
Photo: Meghan Rosen |
UC Santa Cruz graduate student Kingsley Odigie.
(Click on image to see larger version) |
|
|
Odigie, a tall Nigerian with a gentle handshake, stabs his finger at a black-and-white graph on a paper printout. “Leaded gasoline used in California falls right here,” he says, pointing to two circles labeled with industrial sources of lead. His samples carry the combusted remnants of leaded gas. Eventually, rain will flush the ash out to sea. However, it could take centuries to wash all of the lead from California’s Central Valley to the San Francisco Bay. In drier areas, like Los Angeles, lead could stick around even longer.
But the main source of childhood lead exposure in the U.S. lurks closer to our homes: paint. Though lead-based paints were banned in 1978, they still color one-third of U.S. houses.
How many paint flakes would a child have to eat to be in danger? “Not a lot,” says Renee O’Brien, the public health nurse for Santa Clara County. “A little goes a long way.” Just one flake of paint the size of a pencil eraser tip swallowed daily for a few weeks could poison a child, estimates the U.S. Consumer Product Safety Commission. That figure is based on paint with 1.5% lead content. New standards are more than 100 times stricter, but dust from pre-1978 paint still dwells in older, low-income housing.
“Young kids who eat paint or dirt around those homes can get lead poisoning,” says Robert England, the lead surveillance coordinator for San Benito County. But, he notes, lead exposure can happen to anyone. Public health officials have tracked the metal to ceramic glazes, makeup, and even children’s candy. Lately, he says, California regulators have sent consumer safety alerts to his office about candies made in Mexico and India. “We even got one from Australia about licorice,” he says.
The CDC and the California Department of Public Health post online warnings about lead-contaminated foods and list guidelines on how to clean up old paint. However, in countries without such protections, lead poisoning is more common.
 In Flegal’s office, a black frame leans against the side of his desk. It’s a smaller version of his trophy case, with three pictures stacked horizontally. In the center, a 4-year-old boy and his mother smile into the camera. His grin is bright; hers is weary. Beneath them, smokestacks loom over the Australian smelter town where they live. The top photograph captures the same view of the town at dusk, when the stacks bellow fiery clouds into an indigo sunset. Flegal calls the sight “scary beautiful.” In Flegal’s office, a black frame leans against the side of his desk. It’s a smaller version of his trophy case, with three pictures stacked horizontally. In the center, a 4-year-old boy and his mother smile into the camera. His grin is bright; hers is weary. Beneath them, smokestacks loom over the Australian smelter town where they live. The top photograph captures the same view of the town at dusk, when the stacks bellow fiery clouds into an indigo sunset. Flegal calls the sight “scary beautiful.”
He visited the family three years ago during a trip to Mount Isa, a mining city in Queensland that’s shot through with rich veins of copper, silver, and lead. Flegal points to a spot on the picture next to the stack: the family’s home. He moves his finger over a fraction of an inch: the town’s grammar school. The town’s poorest residents live closest to the smelter, where lead concentrates in the air and dirt. Flegal measured the lead in the boy’s blood and in two other children from the town. All three were between 25 and 50 mcg/dl. Double that can kill a kid.
The mines deny their industry is harming anyone. “They say it’s not a problem because all the exhaust goes off over the Pacific Ocean and doesn’t fall over the local community,” Flegal says. Does he think they’re wrong? “Of course!” he exclaims. Families from the town are suing the mining companies and the Queensland government for not warning them about lead dust that belches from the mines, sticks to workers’ boots, and rides on the wheels of vehicles and equipment. The cases have been in litigation for years.
And the boy in the picture? “His IQ is really, really low,” says Flegal. “He’ll always be tweaked.”
Element of risk
At high concentrations, lead’s effects on the body are obvious. It muddies the mind almost like alcohol. Lead-poisoned adults are clumsy and confused, their reactions are slow, and blank spots pockmark their memory. But unlike alcohol, lead can reach beyond the brain and grasp at a person’s hands and feet too. A classic sign of exposure is “drop wrist” or “drop foot,” where the hands and feet dangle limply from the wrist or ankle, fingers and toes stilled by lead-frozen nerves. A similar affliction strikes birds: Thousands of rare Pacific albatross have died of “dropwing” from eating paint chips near rundown U.S. Navy buildings on Midway Atoll.
In kids, exposure to any amount of lead is harmful. Because young digestive systems are especially porous, lead can slip through the walls of a child’s gut and leak into the bloodstream. Once there, lead sneaks into the brain and soaks into the bones. It lodges in the skeleton for decades, biding its time until blood lead levels wane or aging bones begin to crumble. It then trickles out again, creeping back into the bloodstream. Lead’s half-life in blood is 35 days. In living bones, it’s decades.
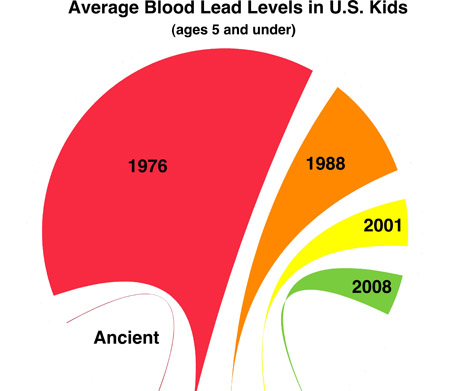 Illustration: Meghan Rosen
Illustration: Meghan Rosen |
A chart of changes in average blood lead concentrations (micrograms per deciliter) in humans, starting with 0.016 in ancient times. Levels soared during the peak leaded gasoline era, to 15 in 1976. They declined to 3.5 in 1988, then 1.6 in 2001 and 1.4 in 2008. Sources: EPA, New England Journal of Medicine. |
|
|
Lead’s effects are most damaging to the central nervous system. “There doesn’t appear to be any lower threshold for lead’s effect on cognition and IQ in children,” says Donald Smith, a metal toxicologist at UC Santa Cruz. He says the evidence is beyond compelling; it’s incontrovertible.
Lead sculpts the shape of brain cells, often by pruning the dendritic branches that reach out to chatter with neighboring cells. In lead-exposed kids, this compels brains to develop networks with eccentric links. “You end up with a different map of connections that alters the ways cells communicate,” Smith says. These detours may make it harder for messages to pass between cells. A 2009 study from California’s environmental health hazard office estimated that raising blood lead levels by just 1 mcg/dl could lower the IQ of an average California kid by one point. Even such tiny changes can nudge a population’s average IQ downward.
But it’s not just about IQ, says Deborah Cory-Slechta, a neurotoxicologist at Rochester University in New York. Lead-exposed children also tend to behave impulsively. In one of her experiments, kids slide digital balls across a computer touch screen to match a preset pattern. It can take five moves to rearrange the balls correctly. “You have to sit back and figure it out first,” Cory-Slechta says. Lead-exposed kids don’t do that. They just start moving balls around.
In kids with severe exposures, chelation therapy—which uses claw-like molecules to grab heavy metals—can help scavenge lead from the blood. But it doesn’t seem to turn back lead’s effects on the brain. Besides, Cory-Slechta says, “Even if I put you in a lead-safe house, the lead in your bones is going to move back into your bloodstream.”
Cory-Slechta was co-chair of the CDC’s Advisory Committee on Childhood Lead Poisoning Prevention (ACCLPP) work group. The group advised throwing out the idea of a lead “level of concern.” “We can’t find a level that’s safe,” Cory-Slechta says. Instead, they recommended intervention based on blood lead levels of children at about 5 mcg/dl—a level exceeded by 2.5% of kids in the U.S. But, Cory-Slechta cautions, this new value “is not the same as saying that 5 mcg/dl is safe.”
 All but one member of the 12-person panel voted “yes.” The sole dissenter was the ACCLPP chair, George Rhoads, a Harvard-trained physician with a master’s degree in public health. He’s not convinced that low blood lead levels are dangerous. “I can’t get too excited about a 6 [mcg/dl] or an 8,” he says. “We all had levels of 15 when I grew up.” All but one member of the 12-person panel voted “yes.” The sole dissenter was the ACCLPP chair, George Rhoads, a Harvard-trained physician with a master’s degree in public health. He’s not convinced that low blood lead levels are dangerous. “I can’t get too excited about a 6 [mcg/dl] or an 8,” he says. “We all had levels of 15 when I grew up.”
Rhoads thinks studies that link low blood lead levels to lower IQ could be muddled by other factors, such as environment or nutrition. Rather, he says, a convincing study would take families living in a high-lead environment, move some of them into low-lead homes, then compare outcomes for children born into both groups. “It’s not an easy trial to do,” Rhoads admits.
Rhoads still believes it’s important to prevent lead exposure and says the U.S. has reduced lead in people’s blood quite effectively. But, he maintains, going from an average blood lead level of 15 to 1 mcg/dl hasn’t measurably improved our IQ or behavior.
“I very much disagree with that,” says Cory-Slechta. “He was the only one that remained unconvinced.”
Should we worry?
There’s no known antidote for lead exposure, but a few preventive tricks can ease lead’s toxic effects. Most are common sense: Wash your hands, don’t swallow paint chips, and avoid imported canned foods. Another simple tactic is eating a healthy diet: Calcium, zinc, and iron block lead’s invasion of the bones. It also helps to give kids lots of opportunities to learn and play. Lead stunts growing brains; stimulating environments help them thrive.
 Flegal thinks it’s important to keep low blood lead levels in perspective. “You don’t want to traumatize people unnecessarily,” he says. After all, when he measured his own level a few years ago, his number was 17. Flegal grew up in a house with lead plumbing and paint: “I specifically remember eating flakes of lead paint. It was sweet!” Still, he says, the amount of lead in our bodies is 100 to 500 times higher than it was in our pre-industrial ancestors. Flegal thinks it’s important to keep low blood lead levels in perspective. “You don’t want to traumatize people unnecessarily,” he says. After all, when he measured his own level a few years ago, his number was 17. Flegal grew up in a house with lead plumbing and paint: “I specifically remember eating flakes of lead paint. It was sweet!” Still, he says, the amount of lead in our bodies is 100 to 500 times higher than it was in our pre-industrial ancestors.
As for my daughter’s blood lead level, I receive a sparsely worded email about her results a week after the test. The subject line reads: “negative/normal.” Briar’s level is less than 3 mcg/dl. According to federal standards, that's safe. But according to science, it's potentially dangerous. Though I’m relieved her number isn’t higher, I wish the test pinpointed a precise amount. Within the range given, Briar’s level could be zero—or it could be twice the national average.
Perhaps the exact amount of lead in our blood isn’t what’s important. The treatment for minor exposure—good food and mental stimulation—is something we should do for our kids anyway. Maybe we just need to understand that lead’s tarnished tendrils will forever entwine with our lives. At some point, in our industrial world, we’ll all feel its touch.
Story ©2012 by Meghan D. Rosen. For reproduction requests, contact the Science Communication Program office.
Top
Biographies
 Meghan D. Rosen Meghan D. Rosen
B.S. (biology) Northern Arizona University
Ph.D. (biochemistry and molecular biology) University of California, Davis
Internships: Science News (Washington, D.C.); National Cancer Institute (Bethesda, MD)
Most people take years to decide on a career, but I had mine picked out in second grade. When I grew up, I was going to become a professional juror. Listening to people’s stories, examining evidence, untangling truth from fiction—it sounded like the perfect job. There was only one catch: My ideal profession didn’t actually exist.
My dissertation work nearly satisfied my childhood dream. I got to ask probing questions (Can mutant thyroid hormone receptors nudge a cell towards malignancy? How?) and share the answers. (We think so. They tinker with its genes.) But the molecular nitty-gritty of research was missing something I cared about: people.
Now, through writing about science, I get to sort out a story’s facts and meet its characters. I think my second-grade self would approve.
. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
 Justine Shih Justine Shih
B.A. (biology) Texas A&M University
As any other child might, I had changing ideas of what I wanted to be when I grew up—an Air Force pilot, a crime scene investigator, a screenplay writer. But two classes that I greatly enjoyed in high school led me to choose biology for my undergraduate studies. With a lifelong interest in art, science illustration turned out to be the next logical step, and the right one as well.
When I am not creating art, I enjoy playing the piano and video games (not at the same time!). Please take a look at my website for more of my work.
Top |
![]()